|
View MMA Documentary Video Series
|
 |
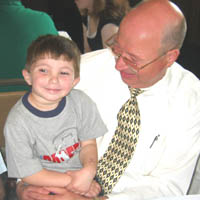
Family Stories; Johnny Tate, Jr. Methlymalonic Acidemia, mut 0, Age 4 The moment our son, John Francis Tate, Jr., was born on January 20, 2000, and placed in my arms, he looked beautifully perfect. Complete joy, total peace, and gratitude filled us. Our tiny angel was finally here. Best of all, my then ten-year-old daughter, Morgan, got to hold her little baby brother. That night after everyone left, I noticed that Johnny was breathing hard. I dismissed it and just thought he was exhausted from nursing. Into the next day, his breathing was still labored. His chest caved in with every breath. Our terrifying and surreal struggle was about to begin. We called our pediatrician and waited. He was not getting better. I called our doctor several times repeating my concerns when finally a NICU doctor took us aside. We later learned that he was in a metabolic crisis and was wheeled into the NICU nursery. Five days later were informed that he had an organic acidemia. This was discovered through his newborn screen. Later on we learned it was Methylmalonic Acidema, mut0. The transport team from Children's Hospital of Philadelphia (CHOP) arrived to take us to where the metabolic doctors could take over his care. Johnny slept on the way over bundled up in his high tech bassinet. John, my husband, followed the transport ambulance in his car and I rode in the ambulance. That was the first time since he was born that we were alone with our fears and prayers. And we both lost it. Johnny spent two long weeks in the NICU at CHOP when he was finally allowed to go home. His levels had stabilized and he was drinking the special medical formula (although very slowly). We were discharged after receiving training on how to place a naso-gastric (ng) tube in our infant son. We thought the training was part of their routine at the hospital since he did not need an ng tube while there. No way, we thought, would we ever have to use one of ‘those' things. At three months, Johnny was tolerating only smaller and smaller feeds. During one feeding, I counted eight little bottles each with a different flavoring that I had tried and Johnny refused. He looked frail and didn't smile much. The day before his christening, we had to resign to finally using the ng tube. It was gut wrenching to actually place the tube down his nose, throat, and into his stomach, then attach the end coming out of his nose to his cheek with tape. He still would not eat on his own even after getting his feeds more consistently. He vomited often. Without notice, Johnny would yank out the tube with his little fist, which meant we had to do the awful insertion procedure again. We finally had to resign to putting in a permanent feeding tube (g-tube). He had the g-tube surgically placed at CHOP. A few days later we went home, with our baby having a long thick tube coming out of his belly. With this device, we were able to bolus feed him around the clock. He did look better, but was still vomiting, sometimes violently. We later concluded, looking back, that it was due to problems with tube and feeding him too much at once. He obviously had capacity issues and was diagnosed with reflux. Johnny is now four years old and still has the g-tube in place. He receives 100% of his nutrition this way. His oral motor and swallowing functions are normal. On a few days out of the month, he will eat a few bites of mini marshmallows or an animal cracker. While he really enjoys the taste, he stops and says he has had enough. We try every day with the guidance of feeding therapists to offer the “ideal” foods in the “ideal” setting to outwit his defenses. It can be depressing when we try to sit as a family to have dinner only to watch him become frustrated, then beg to go watch TV instead. Johnny gets fed every two hours during the day with a medical formula (Propimix-1 and Pro-Phree) plus milk that contains all of his dietary needs. We keep a daily log of each feed, medication, times, and his behavior. For his feeds and medications, we have Johnny sit still so we can administer these through his tube eight to ten times a day. Getting an active four year old to stop what he's doing for the feeds takes patience and creativity. To Johnny's credit, he goes along without any fuss as long as he is doing something he enjoys, like watching TV, playing a game on the computer, or reading a book with his Dad. When we go out, we carry our supplies in a soft-sided cooler with many compartments, to hold his food, meds and supplies. Our care for Johnny has three major parts. One has to do with following his strict diet. The other is has to do with taking care to prevent unnecessary illness. The third part involves monitoring his amino acid levels along with other labs to make sure his nutrition/growth is on target and that his liver and kidney functions are normal. Childhood illness is part of growing up, but for Johnny we do try to avoid “unnecessary” illness because it could cause him to go into a crisis. So we take simple precautions like finding out if anyone is sick before visiting friends or relatives and wash his hands often. It seems like he can weather colds, but GI bugs are different. The day before Easter one year, he caught the Rotavirus bug. At 5:00 pm, he threw up and could not tolerate even 10 ccs. of water later on. By 6:00 pm we were en route to the local ER. By 11:00 pm, right before our eyes, even with IVs he went into a metabolic crisis. Bicarb, which buffers high acid had not been given to him because the lab results on his bicarb levels “weren't back yet.” Meanwhile, Johnny fell asleep and his breathing became eerily strange. We got nervous. We insisted and got the bicarb levels, yet he had already started decompensating. An emergency transport team from CHOP was called to take him where he was in intensive care for three days. He was in for about nine days total, during which time his IV line for TPN failed and infiltrated the tissue in his hand. Our nerves stood on end during that hospital stay, because we also were concerned that he would catch another bug while hospitalized. Already, medically fragile, he has potentially a much tougher time fighting illness because of the MMA. The nightmare of MMA is that sickness could cause us to lose Johnny as we know him. Without urgent care, he could fall into a coma, suffer a stroke or worse. We just don't know which illness will strike or, if it will ever strike at all. We just know that we need to react fast when he gets sick by calling our metabolic doctors right away, especially with viruses that include fever or vomiting. Through all of this, Johnny has been so brave. He bears his disorder with true grace. He rarely complains about how he feels. Even during the worst times, he goes along with our help and sings the ABCs through his tears with us when they need to place an IV. He amazes hospital staff with his courage and outgoing, talkative personality. At home, watching Johnny play is delightful because he has learned to run like the wind, despite having low muscle tone in his legs and really flat feet. He has the most challenge coming down stairs. Like any four year old, he loves going to the park to play alongside other kids. Being very social, he is not shy and he approaches adults with a wave and “Hi!” He tires easily and will simply sit or do less physically challenging play. His cognitive ability is slightly ahead of schedule, which we kind of suspected since he we've seen that he has a terrific memory and a great sense of humor. He gets occupational therapy, physical therapy, and feeding therapy. Next year will be his first year in a small preschool. Without fail, he makes us smile and laugh every day. He is delightful, happy and optimistic. He'll often say upon waking “It's a beautiful sunny day.” He and his fourteen-year-old sister, Morgan, crack each other up even though he drives her crazy at times. Like when he runs to her room to go through the knick-knacks or takes things and puts them in weird places for “safekeeping” like down the heating vent or in the dishwasher. Our life with Johnny is especially precious. We have a child with a life threatening disorder we manage daily. But much more than his physical self, we have him; he is the sweetness and joy of our lives. And, we are very blessed to have our prayers answered in so many ways; for the wisdom of his doctors, the protection and recovery from devastating illnesses, and for his grandparents, aunts, uncles, and especially his cousins, who all love him so very much.
|
|